|
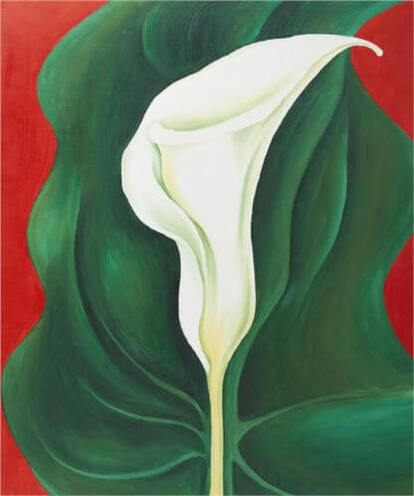
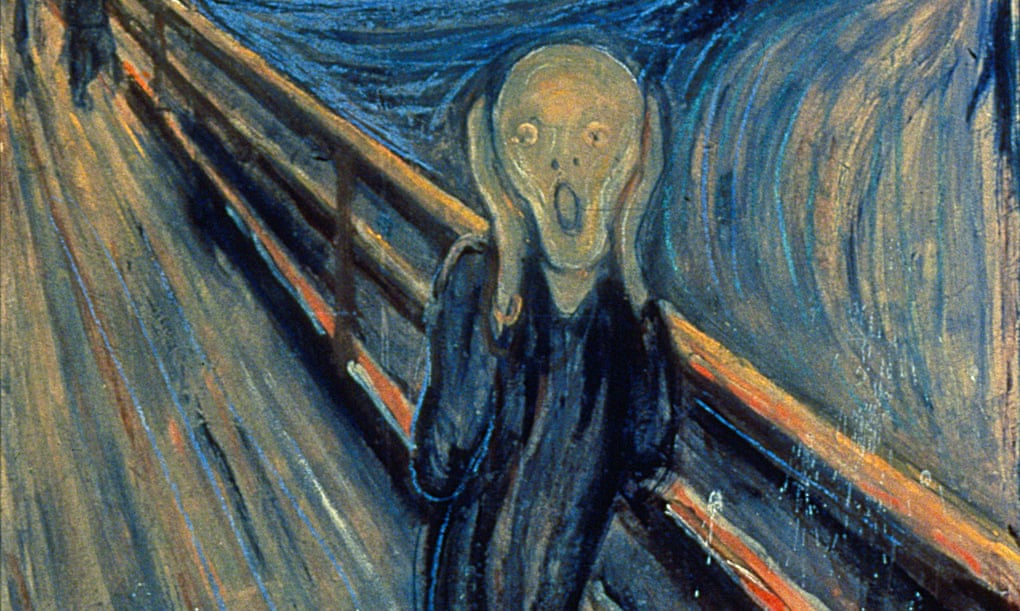
When we think of "therapy", we tend to visualize talk sessions with a qualified therapist. Sitting on the proverbial couch, we spend hours exploring past experiences and learning new tools to deal with future challenges, possibly armed with a fast-depleting box of tissues. But the concept of therapy is much broader. Ever put on a favorite song and feel comforted by its familiar notes? Then you already use music as therapy. If we only learn to appreciate them in the right way, a wider gamut of art - including literature and the visual arts - can also provide solace. Art is therapeutic when it chimes with our inner selves. That favorite song you play has resonance because it recalls deeper insights that can too often be crowded out by intrusive, anxious thought. In highfalutin terms, it speaks the language of your soul. To elicit the benefits of art as therapy, we need only bootstrap our soul's vocabulary. In that spirit, let's explore three works of art that recall important insights when viewed in the right way. Insight #1: Life is messy, and that's OK. Great anxiety arises from the many conflicting demands on our energy, all of which seem at once extremely important and yet stubbornly irresolvable. The ensuing aggregate stress stands in contrast to our dim recollection of a more peaceful childhood, when the most vexing dilemma might have been which flavor ice cream we desire on a hot summer's day. Stoic philosophy flips this anxious thought on its head: the aberration is not our present-day pickle, but instead the impossible simplicity of the child's bubble-wrapped world. That insight is strangely comforting, because it reminds us not to be shocked or dismayed when reality turns out to be rather more bitter than plain-vanilla; it was naive to imagine that things could ever have been otherwise. Art can remind us of this stoic insight. Entitled "Mixed up model", the painting below is composed by the mysterious Proudfoot brothers from New York. The defaced image mirrors the colorful complexity of our present reality. Life's journey is a unique chance to explore, understand and ultimately accept that messy complexity. Insight #2: Even if you're alone, you're not alone. Another therapeutic function of art is to serve as a companion to our woe. Ironically, the artistic portrayal of cognitive frailty can be uplifting, because it reveals that our own troubles are not some faulty aberration of nature: they are instead a reassuringly common feature of the human condition. The painting below is taken from a series of works by British artist James Green, wryly termed "self-portraits of somebody else". It hauntingly depicts confusion and even torment; yet by witnessing these sensations externally our own confusion and torment is shared and therefore lessened. Insight #3: Beauty is in the little things. The therapeutic value of art lies not just in projections of complex realities and shared suffering. Art also serves to remind us of beauty in the little things; those things too often overlooked in the frenetic 21st-century. Born in Wisconsin, the feminist icon Georgia O'Keeffe pioneered modernist art in the United States with abstract impressions of nature. In the painting below, she invites us to admire the understated elegance and bold color of a single lily. That a simple thing can convey such depth of beauty is an enduring source of hope. Care to share? The richness of art is that every piece has therapeutic value by serving as a reminder of some deep insight. We'd love to hear your own stories of therapy through art, so why not send us a message with some favorite art of your own? If you'd like to read more about art as therapy, check out the book by John Armstrong and Alain de Botton (link), which popularized the idea of viewing art this way.
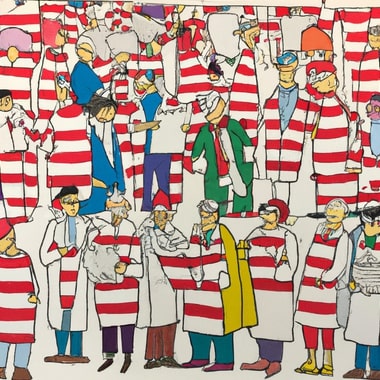
So you've decided to see a psychiatrist. Good on you - that's a big step towards getting better. Take a moment to congratulate yourself. But where are the psychiatrists? Unfortunately, there is a growing shortage of psychiatrists in the United States. Demand for psychiatric services is increasing, partly due to greater awareness of mental health's importance, but the psychiatrist population - currently about 35,000 nationwide - is actually falling as older providers retire (see post). The shortage of psychiatrists is a big social problem - and it also presents a challenge for the individual seeking great care. At times, it might even feel like a "Where's Waldo?" game - you're vainly trying to find a great psychiatrist among a bunch of look-alike pretenders. Seek, and you shall find. The national shortage of psychiatrists means that you might need to put some extra effort into finding the right provider for you. The first step is to figure out the right clinical setting. If the concern is urgent, an emergency room or urgent care clinic is most appropriate. In most cases, however, an out-patient clinic is the way to go. Cost-conscious patients can try to seek care from a local community clinic or find a provider who is in-network with their insurance carrier. Unfortunately, however, the availability of such providers is limited. Psychiatrists who accept insurance may also be more time-constrained as they typically see more patients per day.
Here's a handy stepwise guide for finding the right out-patient provider:
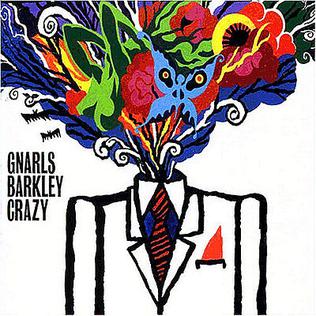
"Does that make me crazy?" Thus asks CeeLo Green in the crescendo of soul duo Gnarls Barkley's pop hit, "Crazy". It's a groovy tune, but a responsible psychiatrist - maybe after showing off a few dance moves - should retort: "No, it doesn't. And by asking the question, you're trivializing mental illness." And yet the song goes on:
… I remember when I remember, I remember when I lost my mind There was something so pleasant about that place Even your emotions have an echo in so much space … And when you're out there without care Yeah, I was out of touch But it wasn't because I didn't know enough I just knew too much … Does that make me crazy? Does that make me crazy? Does that make me crazy? Possibly!
Such lyrical over-reach trivializes mental illness by minimizing its consequences. In the song, CeeLo Green rhetorically asks whether he is "crazy" because he "knew too much" and was "out of touch". This seemingly innocent misuse of the word "crazy" is perpetuated in casual language, where it can refer to anything that deviates from middle-of-the-road conventionality. Such definition creep - the origin of the word crazy is in something diseased, sickly, or broken - risks trivializing genuine mental illness.
Similar trivializations of mental illness in casual language are rife. Here are a few more examples that crop up in day-to-day speech:
Mindfulness about the appropriate choice of words is not a form of censorship. Freedom of speech is essential to a well-functioning society and should be protected, as indeed it is in the US Constitution. But any freedom comes with responsibility. We are not entering some Orwellian dystopia by being more aware of how language shapes impressions of mental illness. Instead, the hope is that - with greater mindfulness in our choice of words - maladies of the brain will eventually come to be treated in society with the same level of seriousness as maladies afflicting other organs. Once we've achieved that level of collective enlightenment, we can reward ourselves with a celebratory dance to Gnarls Barkley's groovy tune. Just be mindful of the lyrics! Health insurance companies maintain networks of medical providers, which offer services at pre-negotiated rates. These networks promise predictability in expenses for the insurance company, but limit choice for patients and can constrain access to effective health care.
Patient choice is hampered when networks are small. While insurance companies advertise impressively long lists of providers who are in-network, some of these providers may have long waiting lists or be closed to new patients. Even worse, they may have ceased their relationship with the insurance company or stopped practicing altogether. The latter case is what's known as a "ghost network" of providers nominally listed as in-network, but who are not in fact available to provide in-network services. Ghost networks are particularly widespread in behavioral health. In two recent studies (see here and here) run by J. Wesley Boyd, a professor of psychiatry at Harvard Medical School, researchers contacted several hundred psychiatrists listed by Blue Cross Blue Shield as in-network providers. Of these, only about one-quarter were actually accepting new adult patients. Three-quarters were "ghosts" - either unreachable or not accepting new patients. Insurance companies should be required to actively maintain lists of in-network providers. Inflating networks by not removing unavailable providers exaggerates the benefits of an insurance policy and misleads patients regarding their access to care. Fortunately, state authorities in California and Massachusetts have taken action against certain insurance companies that fail this basic duty. The hope is that this issue grows in salience as a matter of national importance.
Benjamin Rush is the founding father you might never have heard of. In 1776, he represented Pennsylvania in declaring the new nation formally free of regal tyranny. Seated in his hometown alongside more famous comrades like Thomas Jefferson, John Adams, and Benjamin Franklin, Dr. Rush declared a new, independent United States.
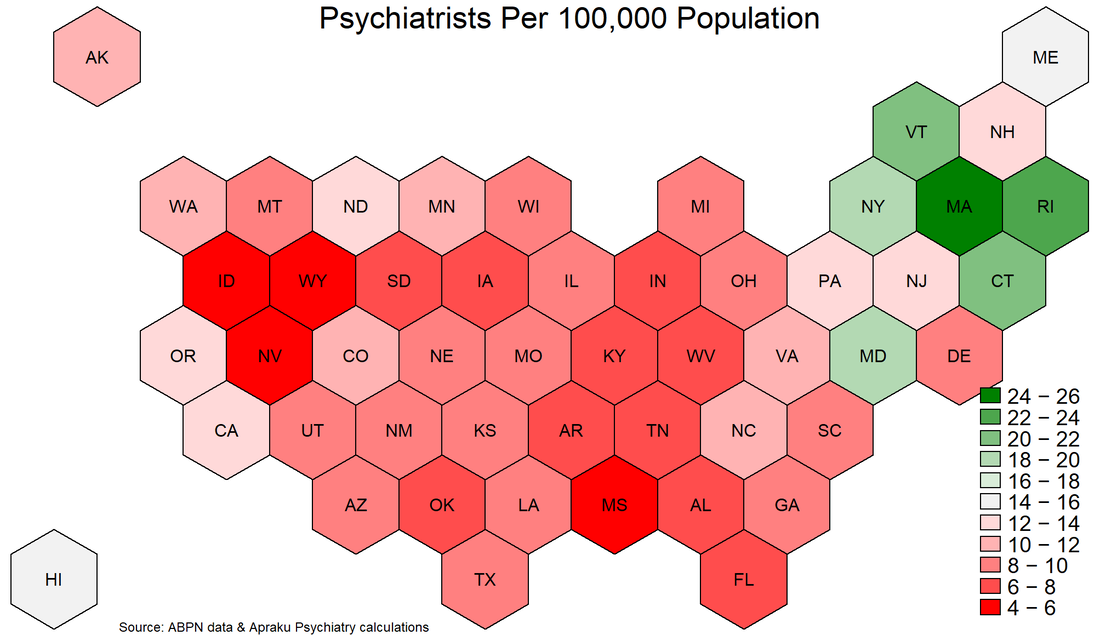
But Dr. Rush not only fathered a new country. He also fathered something of perhaps even longer-lasting importance for humanity: the medical specialty of psychiatry. Yes, Dr. Rush is the father of psychiatry – and that's according to its U.S. custodian, the American Psychiatric Association. In this blog post, we'll dive into the fascinating story of this unsung hero, exploring his rise to prominence, groundbreaking medical innovations, and the powerful legacy he left behind. Strap in for a captivating journey through the life of the man known as the "Father of American Psychiatry." From Tragedy to Triumph: Benjamin Rush's Early YearsBorn in 1746 in a rural community just outside Philadelphia, Benjamin Rush was a child prodigy who overcame personal tragedy to shape the future of medicine and politics. When Benjamin was just six, his father passed away, leaving his mother, Susanna, to raise seven children. Despite this personal tragedy, Susanna made sure her children received the best education possible. At the age of eight, Benjamin was sent to study under his uncle, Dr. Samuel Finley, headmaster of Nottingham Academy in Maryland. This rigorous education fueled his passion for learning, and by 13, he was enrolled at the College of New Jersey (later Princeton University). Proving his brilliance, he graduated with a Bachelor of Arts degree at only 14 years old. Benjamin returned to Philadelphia to apprentice under Dr. John Redman. This hands-on experience exposed him to various medical practices and ignited his interest in psychiatry. Seeking the best medical education, he ventured to the University of Edinburgh, a prestigious institution known for its groundbreaking research. Studying under renowned professors like Dr. William Cullen and Dr. Joseph Black, Benjamin absorbed cutting-edge ideas that would later define his innovative contributions to psychiatry. Returning to America with his medical degree, Benjamin Rush embarked on a journey that would forever change the landscape of medicine and American history. Pioneering Contributions to PsychiatryBenjamin Rush's pioneering contributions to psychiatry revolutionized the way society understood and treated mental illness. He challenged conventional beliefs and advocated for humane care, laying the groundwork for modern psychiatry. Thanks to his innovative spirit and tenacity, Dr. Rush earned the title "Father of American Psychiatry." At a time when mental illness was often viewed as a moral failing or divine punishment, Rush made the audacious claim that it was a medical condition deserving of compassion and treatment. He believed that mental disorders stemmed from physical causes, shattering the stigma surrounding these conditions. This groundbreaking insight marked a significant shift in society's perception of mental illness and paved the way for more effective treatments. Dr. Rush's unorthodox approach to psychiatry led to the development of novel treatment methods. He championed the use of tranquilizers, which he believed could calm patients' minds and alleviate their symptoms. He also invented the "tranquilizing chair," a revolutionary device that restrained patients without causing harm. This chair allowed patients to safely experience their emotions while being treated with dignity and respect. While these innovations were broadly ineffective, they represented an experimental, scientific approach to medicine that ultimately led to the effective psychiatric treatments that are in use today. Another key aspect of Dr. Rush's innovative approach to psychiatry was his emphasis on the importance of physical activity for mental well-being. He encouraged patients to engage in regular exercise and work therapy, advocating for the therapeutic benefits of fresh air, sunlight, and a structured daily routine. This holistic approach to mental health care was years ahead of its time and continues to influence modern psychiatric practices. Rush's influence also extended to the design and administration of mental health institutions. He advocated for the creation of separate wards for patients with mental illness, ensuring they received specialized care. He also pushed for the training of medical professionals in psychiatry, which contributed to the development of the field as a distinct medical specialty. The impact of Benjamin Rush's pioneering work in psychiatry cannot be overstated. He tore down age-old misconceptions and replaced them with a compassionate, scientific understanding of mental illness. In doing so, he not only revolutionized psychiatric care but also made lasting contributions to the medical profession and society as a whole. Dr. Rush's trailblazing spirit remains an inspiration for those committed to improving mental health care and breaking down the barriers that still exist today. Political Involvement and Founding Father StatusBenjamin Rush was a medical pioneer, a trailblazer in psychiatry, and a Founding Father with fiery political convictions. He played a crucial role in shaping the early United States, leaving an indelible mark on the country's political landscape. As a signer of the Declaration of Independence, Rush stood shoulder to shoulder with iconic figures like Thomas Jefferson, John Adams, and Benjamin Franklin. Together, they proclaimed the new nation's freedom from British tyranny. Dr. Rush's unwavering commitment to the revolutionary cause led to his appointment as Surgeon General of the Continental Army. He fearlessly tended to the wounded in the midst of the American Revolution, displaying courage, dedication, and skill under immense pressure. Rush not only contributed to the birth of the nation, but he also actively participated in shaping its institutions. He played a key role in founding Dickinson College and the Philadelphia Dispensary, demonstrating his commitment to education and public health. Benjamin Rush was a man of strong convictions, unafraid to take a stand on controversial issues. He was an ardent abolitionist, passionately advocating for the end of slavery. Additionally, he championed women's rights, paving the way for future generations to enjoy greater equality. This Founding Father's political involvement and unwavering dedication to the revolutionary cause, coupled with his groundbreaking work in psychiatry, make Benjamin Rush a captivating and inspiring figure in American history. His legacy continues to resonate, reminding us of the immense potential for change when passion, innovation, and conviction converge. Controversies and LegacyBenjamin Rush was a revolutionary figure with a legacy as multifaceted as the man himself. While his pioneering work in psychiatry and his dedication to the United States' founding principles are undeniably commendable, his story is not without its fair share of controversies. Rush's staunch advocacy for bloodletting as a medical treatment, for instance, was a point of contention among his peers. Despite his unwavering belief in its efficacy, history would later prove the practice to be more harmful than helpful, casting a shadow over his medical career. Similarly, Rush's opinionated nature and outspokenness occasionally stirred up controversy. His fiery convictions on topics like slavery and women's rights, while progressive for his time, sparked heated debates and drew both admirers and detractors. Yet, despite these controversies, Rush's enduring legacy cannot be denied. His tireless efforts in advocating for the humane treatment of people with mental illness laid the groundwork for modern psychiatry. His insistence on compassion and understanding in the face of ignorance and superstition has left an indelible mark on the field. As a Founding Father, Rush's political influence shaped the early United States, and his unwavering commitment to its revolutionary cause will forever be etched in history. His involvement in establishing important institutions like Dickinson College and the Philadelphia Dispensary underscores his dedication to education and public health. In the grand tapestry of American history, Benjamin Rush stands out as a vibrant, complex, and inspirational figure. His controversies, in many ways, only serve to make his story more intriguing, and his legacy more fascinating. A testament to the power of passion and conviction, Rush's contributions to medicine, politics, and social justice continue to echo through the ages. The United States has a severe and growing shortage of psychiatrists. While demand for mental health services is rising, the pool of psychiatrists is shrinking: graduating residents are too few to replace new retirees. The Department of Health and Human Services estimates the shortage of adult psychiatrists to reach 12,500 by 2030, representing nearly 50% of psychiatrists nationwide. Unfortunately, the current situation is perhaps even worse than described by the DHHS. For starters, the DHHS assumes that all psychiatrists work until age 75, which seems overly optimistic about enthusiasm for late-life work. Moreover, the DHHS report uses a dataset maintained by the American Medical Association, which records physicians' self-designated primary specialty. However, self-designation does not necessarily mean that a physician has expertise or Board certification in psychiatry. Finally, AMA records are often not kept up to date by physicians, as this is not required for licensing purposes. To better gauge the availability of qualified psychiatrists, we can use data from the American Board of Psychiatry and Neurology. Active certification by the ABPN is the gold standard in psychiatry. We further restrict the data sample to Board-certified psychiatrists who were initially certified between 1988 and 2019 (psychiatrists certified before 1988 are assumed to have retired, consistent with a retirement age of 65). The ABPN data indicate that there are just over 35,000 Board-certified psychiatrists of working age in the US. This stands in contrast with the figure of approximately 42,000 estimated by the DHHS, suggesting that the current shortfall in psychiatrists may be twice as large as previously reported. Most of the discrepancy arises from DHHS's assumed retirement age of 75 rather than 65, while the remainder comes from the fact that the DHHS relies on physicians' self-designated specialty, rather than their Board certification. The ABPN data also contain information on the primary city in which psychiatrists practice. This allows for in-depth analysis of geographic dispersion in availability. As a first step, we can plot the state-level distribution of psychiatrists per 100,000 population (see graph below). According to the DHHS, demand for psychiatric services requires a supply of approximately 15 psychiatrists per 100,000 population. Just six states - MA, RI, VT, CT, NY, MD (in descending order) - comfortably exceed this threshold; the vast majority of US residents therefore live in a state in which the psychiatrist-population ratio is inadequate according to DHHS estimates. Worryingly, 14 states have a psychiatrist-population ratio which is less than half of that which the DHHS deems adequate. What can society do about this psychiatry shortage? To answer this question, it is important to distinguish two aspects of the problem: aggregate shortage and geographic dispersion.
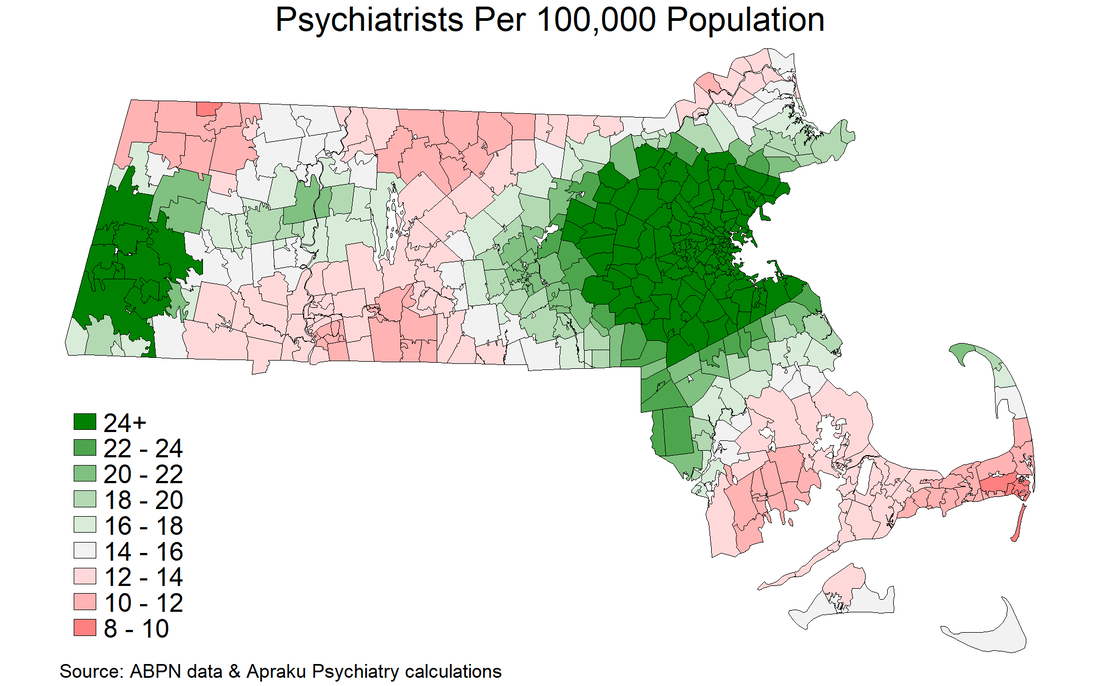
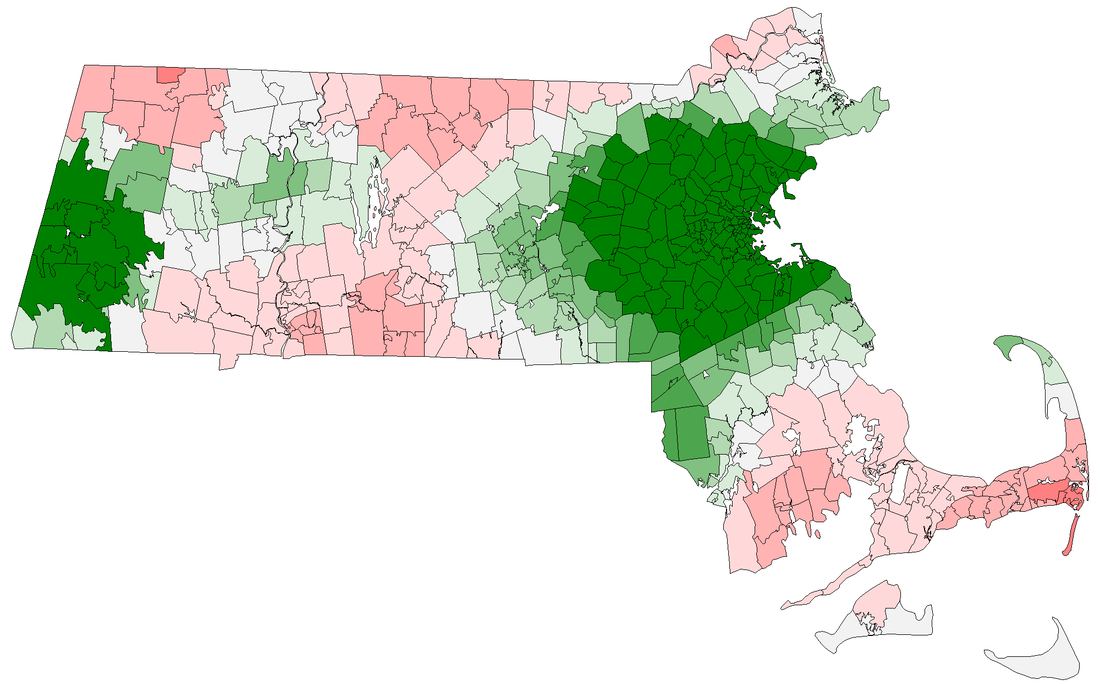
To address aggregate shortage, there is only one answer: get more psychiatrists! Over the long run, an expansion in residency training programs would help to increase the rate at which retiring psychiatrists are replaced. In the shorter-run, a more liberal immigration policy and licensing regime with respect to foreign-trained psychiatrists would help alleviate scarcity. These solutions are preferable to lowering standards of care, for example by expanding the ability of nurse practitioners to practice independently. In general, foreign-trained psychiatrists follow a more rigorous curriculum than US-trained nurse practitioners. There are multiple solutions to the geographic dispersion problem. The most readily implementable involves greater adoption of tele-medicine, as practiced by Apraku Psychiatry, which can alleviate within-state scarcity. Unfortunately, state-level regulation of physician licensing impairs the ability of tele-medicine to alleviate cross-state scarcity, although the Interstate Medical Licensure Compact may be somewhat helpful in reducing frictions in this respect. In the longer-run, a strategic geographic reallocation of psychiatry residency programs could help to expand coverage in under-served areas. Some provisions in the Affordable Care Act (2010) went in this direction, but the analysis shown here underscores the need for a more extensive overhaul. Massachusetts has the most psychiatrists per capita among US states. There are approximately 1,700 Board-certified psychiatrists of working age whose primary practice location is in Massachusetts. This gives the state 25 psychiatrists per 100,000 population - more than double the national average of 11. Yet psychiatrists in the Bay State are heavily concentrated around Boston. About two-thirds are based within the I-95. Consequently, Massachusetts residents living outside of this bubble are less well served than the state-level average would suggest. The map below plots the psychiatrist-population ratio at zipcode level. In addition to many rural communities, the city of Springfield in central Massachusetts, as well as Haverhill, Lawrence and Lowell in the north-east, are relatively poorly served, with psychiatrist-population ratios below the level deemed adequate by the Department of Health and Human Services. Across Massachusetts, nearly two million people live in a zipcode with a below-adequate psychiatrist-population ratio. Thus, Massachusetts' number-one ranking among states should not be cause for complacency regarding the provision of mental health services. To alleviate local shortages, a more widespread use of tele-psychiatry can be effective in granting local populations access to out-of-town psychiatrists licensed in the state. In this way, tele-psychiatry can grant all Massachusetts residents the benefits of the state's relatively ample supply of psychiatrists - not just those who happen to live in the Boston area.
The path to becoming a psychiatrist is long, requiring more than a decade in higher education. It starts with an undergraduate degree in which prospective psychiatrists often follow a "pre-med" sequence of courses that includes biology, chemistry, physics and math. Then comes medical school, which is a four-year journey comprising classroom learning, several day-long exams and a series of clinical rotations providing practical exposure to medical specialties. Yet graduation from medical school is just the "end of the beginning". After setting their sights on psychiatry, a freshly minted medical doctor must obtain admission to an accredited residency program. There are approximately 250 such programs in the United States. These four-year programs combine on-the-job training with specialized teaching in psychiatric science by professors in psychiatry. Upon graduating from such a program, physicians will have gained experience across the full range of psychiatric practice, from in-patient settings featuring patients with acute mental disorders to out-patient clinics in the community or college campuses.
Finally, after at least 12 years of intensive study and clinical practice, a would-be psychiatrist's training culminates in an eight-hour examination. Set by the American Board of Psychiatry and Neurology, this exam covers the full range of subject matter that psychiatrists are expected to master. Only after passing this exam can a physician claim to be Board-certified in psychiatry. The ABPN certifies about 1,500 new psychiatrists each year. This is actually slightly less than the number of psychiatrists retiring each year, which is why the United States faces a growing psychiatrist shortage.
Have you ever considered how your daily commute or long drives might be impacting your mental health? While driving might be convenient and, at times, enjoyable, it can also lead to stress, anxiety, and other mental health concerns. In this blog post, we'll explore the various ways in which driving can negatively affect mental well-being and provide some suggestions on how to cope with these challenges.
The Connection Between Driving and StressDriving is an activity that many people engage in on a daily basis, whether it be for work or personal reasons. However, it can also be a significant source of stress that can have a negative impact on our mental well-being. There are several factors that contribute to the stress that people experience while driving. Driving as a Daily StressorFor many people, driving seems an unavoidable part of their daily routine. Commuting to work, running errands, or taking the kids to school often involve spending considerable time behind the wheel. As a result, these everyday activities can serve as constant sources of stress, taking a toll on mental well-being. The Role of Traffic CongestionOne of the primary causes of stress while driving is traffic congestion. It can significantly increase the time it takes to reach a destination, leading to frustration and a sense of helplessness. Sitting in heavy traffic can also trigger feelings of claustrophobia and irritability, further contributing to stress levels. Over time, repeatedly dealing with traffic congestion can create a sense of dread or anxiety related to driving. The Impact of Aggressive DriversEncountering aggressive drivers on the road can be a major source of stress. Road rage incidents, tailgating, or dangerous maneuvers by other drivers can put both your safety and mental health at risk. These encounters can lead to increased anxiety and even fear of driving, as you may begin to anticipate negative interactions with other motorists. Driving and the Effects on SleepSpending long hours behind the wheel can disrupt our sleep patterns, particularly for those who work irregular hours or drive at night. Insufficient sleep is associated with a range of mental health issues, including mood disorders, impaired cognitive function, and increased risk of developing depression and anxiety. Ensuring that you get enough rest and maintain a consistent sleep schedule is essential for preserving mental health and overall well-being. The Cumulative Effects of Driving StressWhile individual instances of driving stress may seem manageable, the cumulative effects of these stressors can have long-term consequences for mental health. Consistently high stress levels can lead to burnout, a weakened immune system, and an increased risk of developing mental health issues such as depression or anxiety. Furthermore, stress can exacerbate existing mental health conditions, making it more challenging to cope with daily life. Key Insights on the Connection Between Driving and Mental Health
The Impact of Sedentary Behavior and Missed OpportunitiesDriving is a sedentary activity, and long hours spent in a car can contribute to a sedentary lifestyle. Sedentary behavior is linked to an increased risk of developing mental health issues such as depression, anxiety, and overall poor emotional well-being. The Value of ExerciseIncorporating regular physical activity into your routine can help counteract the negative effects of a sedentary lifestyle and promote better mental health. Engaging in physical activities like walking or cycling as part of your daily commute can have numerous mental health benefits. Exercise has been proven to reduce stress, alleviate anxiety and depression, and improve overall mood. Social Interaction and Public TransportationDriving is often a solitary activity or shared with just a few passengers, while taking public transportation or walking can provide more opportunities for social interaction. Engaging with others, even through simple pleasantries, can foster a sense of connection and belonging. Social interaction is vital for maintaining good mental health, as it helps to reduce feelings of isolation and loneliness. The Positive Atmosphere of Alternative Transportation OptionsPeople often experience more pleasant emotions while using alternative transportation methods, as these activities can be inherently enjoyable. Walking or cycling allows you to enjoy the outdoors and take in the scenery, creating a positive atmosphere that can contribute to better mental health. Furthermore, public transport brings opportunities for social interaction, which is also beneficial for mental health. Evidence on the Connection Between Driving and Stress
Tips for Managing the Mental Health Impact of DrivingDriving can have a significant impact on mental health, but there are strategies that can help reduce this impact. Here are some tips for coping with essential driving and adopting alternative transportation options: Coping with Essential Driving
Adopt Strategies to Integrate Alternative Transport Options
By making these small, mindful decisions about your transportation choices, you can create a more positive and healthy balance in your daily life, reducing the negative effects of driving on your mental health. But if you're still struggling with stress, anxiety, or other mental health concerns related to driving, don't hesitate to seek the help of a mental health professional. They can provide guidance and support to help you manage these challenges and improve your overall well-being. ConclusionDriving can have a significant impact on mental health, but there are strategies that can help reduce this impact. In this blog post, we have explored the various ways in which driving can negatively affect mental well-being and provided some suggestions on how to cope with these challenges. By making small, mindful decisions about your transportation choices, you can create a more positive and healthy balance in your daily life, reducing the negative effects of driving on your mental health. Incorporating physical activity and alternative transportation methods into your routine can have numerous mental health benefits, promoting better overall well-being. It is important to remember that these tips are not a substitute for seeking professional help. If you are struggling with stress, anxiety, or other mental health concerns related to driving, discuss your concerns with a psychiatrist. They can provide guidance and support to help you manage these challenges and improve your overall well-being.
Transferring psychiatrists can be a daunting task, but it is essential to prioritize your mental health needs and find the right provider to support your journey. In this article, we'll outline the steps to transfer psychiatrists, ensuring a smooth transition and continued mental health care.
Reflect on your reasons for transferringBefore making any changes, take the time to reflect on your reasons for wanting to transfer psychiatrists. It's essential to have a clear understanding of your needs and expectations, as this can help you find the right fit and ensure a smoother transition. Potential reasons may include:
For more information on these reasons and guidance on when it might be time to find a new psychiatrist, see this related article: Time to Find a New Psychiatrist. Research potential psychiatristsOnce you've identified your reasons for transferring, start researching potential new psychiatrists who can best meet your needs. This process is essential to finding a provider who is well-suited to your specific situation, ensuring a more successful therapeutic relationship. Consider the following criteria when searching for a new psychiatrist:
For further guidance on identifying the qualities that make a great psychiatrist, refer to this article: What Makes a Great Psychiatrist. You may also consider checking out the profiles of psychiatrists at Apraku Psychiatry to find a provider who's right for you. Finally, if you're moving to a new location, be sure to check out the available providers in your state. Schedule an initial evaluation with the new psychiatristOnce you've identified a potential new psychiatrist, the next step is to schedule an initial evaluation. This appointment is crucial for establishing a strong foundation for your therapeutic relationship and ensuring the new psychiatrist fully understands your mental health needs. The initial evaluation typically involves the following:
Finally, remember that open communication is key to building a successful therapeutic relationship. Be honest about your experiences, concerns, and goals during the initial evaluation, and don't hesitate to ask questions. Your active engagement in this process will help ensure the best possible outcomes for your mental health journey. To schedule an appointment at Apraku Psychiatry, simply complete the intake form on our website. Update your current psychiatristIt's important to maintain open communication with your current psychiatrist during the transfer process. Inform them of your decision to switch providers and request that they share your records with your new psychiatrist. This will ensure a smooth transition and help your new psychiatrist become familiar with your treatment history. You may also consider requesting your current psychiatrist to transfer records to your new provider. Transferring records is not mandatory, but it can be helpful for your new psychiatrist to have access to your previous treatment information. If you decide to transfer records, request that your current psychiatrist send them to your new provider. If your new provider is a psychiatrist at Apraku Psychiatry, records can be securely faxed to the practice at (855) 651-0589. Prepare for your first appointment with your new psychiatristEnsuring a smooth transition to a new psychiatrist involves being well-prepared for your first appointment. Taking the time to gather necessary information and organize your thoughts can contribute to a more productive and successful initial meeting. Here are some tips to help you prepare:
Psychiatrists play a vital role in addressing mental health concerns and providing appropriate care for their patients. Occasionally, psychiatrists may offer home visits to patients who cannot or do not wish to visit their office. However, home visits are increasingly uncommon, and tele-psychiatry has emerged as a convenient and accessible alternative. Tele-psychiatry offers the same convenience as home benefits as well as some added benefits, including greater availability and choice among mental health professionals.
The Purpose of a Home Visit in PsychiatryHome visits in psychiatry are intended to provide mental health care to patients who cannot or do not wish to visit a mental health clinic. There are a couple reasons a patient might prefer to be seen at home:
Drawbacks of Home VisitsDespite their potential benefits, home visits in psychiatry also have some disadvantages:
Tele-psychiatry as a Substitute for Home VisitsTele-psychiatry has emerged as a viable substitute for home visits, offering the same level of convenience while also providing greater accessibility and availability. Patients can connect with a wider range of psychiatrists, such as the doctors listed here. With tele-psychiatry, patients can receive mental health care from any location in state with a stable internet connection. This is particularly helpful for individuals who live in remote areas or who have mobility limitations, as they can access care in any one of the states where the psychiatrist is licensed. If convenient, the patient also has the option of connecting from private spaces other than their home, such as a private office or hotel room located in state. Tele-psychiatry also offers patients a wider choice of psychiatrists, such as the psychiatrists available at Apraku Psychiatry. This allows patients to find the right professional to meet their unique needs and preferences. Furthermore, research has shown that tele-psychiatry can be equally effective from a clinical standpoint as regular in-person clinic visits. Getting Started with Tele-psychiatryConnecting with a tele-psychiatrist is a simple process. Patients can follow these steps:
ConclusionWhile home visits are an attractive option for some patients, the availability of psychiatrists is very limited. Tele-psychiatry has emerged as a convenient, accessible, and private alternative to traditional in-person care. With the increased availability of tele-psychiatry services, patients can now receive mental health support from an in-state location of their choosing and connect with a wider range of mental health professionals to meet their individual needs.
Are you considering seeing a psychiatrist for the first time? It's completely normal to feel nervous or uncertain about the process. That's why we've created this comprehensive guide to help you feel more prepared and empowered for your appointment with a psychiatrist, whether at Apraku Psychiatry or elsewhere. With our practical tips on how to make the most out of your visit, you'll be on your way to taking control of your mental health and achieving your wellness goals.
Key Insights on Preparing for and Communicating with Your Psychiatrist
How to prepare for your psychiatrist appointmentKnowing what to expect during a psychiatrist appointment can help you feel more comfortable and prepared. Here are some things you can expect during your appointment:
By following these tips, you can feel more prepared and confident during your appointment. Remember, your psychiatrist is there to help you, and being open and honest with them can help you receive the best possible care. Don't be afraid to ask questions or share your concerns, and be willing to work collaboratively with your psychiatrist to develop a treatment plan that works for you. What to expect during your psychiatrist appointmentKnowing what to expect during a psychiatrist appointment can help you feel more comfortable and prepared. Here are some things you can expect during your appointment:
By understanding what to expect during your appointment, you can feel more prepared and empowered to take an active role in your mental health care. Remember, your psychiatrist is there to help you, and being honest and open with them can help you receive the best possible care. How to talk with your psychiatristEffective communication with your psychiatrist is key to getting the most out of your mental health care. Here are some tips to help you communicate effectively with your psychiatrist:
Effective communication with your psychiatrist is a two-way process. Therefore, always make sure to ask your psychiatrist any questions you may have, especially if something is unclear. This can help you understand your treatment options better and feel more comfortable with the care you're receiving. By following these tips, you can communicate more effectively with your psychiatrist and feel more empowered and in control of your mental health care. Remember, your psychiatrist is there to help you, and effective communication is key to achieving the best possible outcome. Evidence on the Importance of Effective Communication
How to Ask Questions During Your Psychiatrist AppointmentAsking questions during your psychiatry appointment is an important part of understanding your mental health and getting the care you need. Here are some tips on how to ask questions effectively:
By following these tips, you can ask questions more effectively during your psychiatry appointment and feel more informed and empowered about your mental health care. Remember, your psychiatrist is there to help you, and asking questions is an important part of getting the care you need. Conclusion: Super-Charging Your Mental Health CareTaking care of your mental health is an important part of overall wellness. By working with a licensed and Board-certified psychiatrist, such as those at Apraku Psychiatry, you can receive the care and support you need to manage your mental health effectively. Preparing for your psychiatry appointment by following the tips outlined in this article can help you feel more comfortable and confident during your visit. By being open and honest with your psychiatrist and actively participating in your mental health care, you can help ensure that you receive the best possible treatment. Remember, mental health care is a collaborative effort between you and your psychiatrist. By communicating effectively, asking questions, and prioritizing your mental health, you can empower yourself to take control of your mental health care and improve your overall well-being. At Apraku Psychiatry, we are committed to providing our patients with the highest quality care and support. We encourage our patients to implement the tips outlined in this article during appointments with their psychiatrist, and to reach out to us with any questions or concerns they may have. Together, we can work to achieve optimal mental health outcomes and improve quality of life.
Are you curious about Lexapro and its role in treating depression and anxiety disorders? In this comprehensive blog post, we'll explore the world of this popular antidepressant medication, unraveling its mysteries and unveiling crucial insights. Join us as we dive into why psychiatrists prescribe Lexapro, how it works its magic on your brain, and what you need to know about side effects and alternative treatments. Whether you're considering Lexapro for yourself or a loved one, or simply want to stay informed, this post will serve as your ultimate guide to navigating the Lexapro landscape. Get ready and let's embark on our journey!
What is Lexapro and When Do Psychiatrists Prescribe It?Have you been hearing about Lexapro (escitalopram) and wondering what the buzz is all about? You're not alone. Many patients are curious about this widely-prescribed medication. In this section, we'll dive into what Lexapro is, the conditions it's prescribed for, and factors that psychiatrists consider before prescribing it. First things first, Lexapro is an antidepressant medication that belongs to a class of drugs known as selective serotonin reuptake inhibitors (SSRIs). SSRIs are a popular choice among mental health professionals because they typically have fewer side effects than other types of antidepressants. They work by increasing the levels of serotonin—a chemical that helps regulate mood—in the brain. When Psychiatrists Prescribe Lexapro
But how do psychiatrists decide whether Lexapro is the right choice for a particular patient? There are several factors that come into play. First, the psychiatrist will assess the severity of the patient's symptoms and determine whether medication is appropriate in the first place. For milder cases, non-pharmacological treatments, such as therapy, may be recommended first. Next, the psychiatrist will consider the patient's medical history and any co-occurring health issues. Some individuals may have a higher risk of side effects, or their condition might be better managed by a different class of medication. Additionally, the psychiatrist will take into account any other medications the patient is currently taking to avoid potential drug interactions. Lastly, patient preferences play a crucial role in the decision-making process. Some individuals might have had positive experiences with a certain type of medication in the past, or they may be more inclined to try a specific treatment due to personal research or recommendations from friends or family. It's important for psychiatrists to work collaboratively with their patients to find the most effective and well-tolerated treatment plan. In summary, Lexapro is a widely-prescribed SSRI that is commonly used to treat depression, obsessive-compulsive disorder, and anxiety. When considering whether to prescribe Lexapro, psychiatrists assess the patient's symptoms, medical history, current medications, and personal preferences. Stay tuned for the next section, where we'll explore how Lexapro works to improve mood and alleviate symptoms. Top Highlights
How Does Lexapro Work?The Role of Serotonin in Mood RegulationYou're probably curious about how Lexapro actually works to improve mood and alleviate symptoms of anxiety. In this section, we'll delve into the role of serotonin in mood regulation, how Lexapro increases serotonin levels in the brain, and the timeline for the medication to take effect. Increasing Serotonin Levels in the BrainSerotonin is a neurotransmitter, a chemical that facilitates communication between nerve cells in the brain. It plays a critical role in regulating mood, sleep, appetite, and other important functions. Research has shown that an imbalance in serotonin levels is often associated with mental health symptoms. This is where Lexapro comes in. As an SSRI, Lexapro specifically targets serotonin levels in the brain. It works by blocking the reabsorption (or reuptake) of serotonin by certain nerve cells, leaving more serotonin available in the synaptic cleft—the tiny gap between nerve cells. With more serotonin available, communication between nerve cells is enhanced, leading to improvements in mood and a reduction in anxiety symptoms. The Timeline for EffectivenessIt's important to note that Lexapro doesn't provide immediate relief. In fact, it can take a few weeks for the medication to start showing its full effects. This is because the brain needs time to adjust to the increased levels of serotonin. During this period, it's crucial for patients to communicate with their psychiatrist about any changes they experience, as some individuals might need adjustments to their dosage or even a switch to a different medication. Important ConsiderationsAnother aspect to keep in mind is that the effectiveness of Lexapro can vary from person to person. While some individuals may experience significant improvements in their symptoms, others might not find the relief they're seeking. This highlights the importance of maintaining open communication with the treating psychiatrist and being patient while waiting for the medication to take effect. Wrapping up: Lexapro works by increasing the availability of serotonin in the brain, which in turn helps regulate mood and alleviate symptoms of anxiety. It can take a few weeks for the full effects to become apparent, and the response to the medication can vary between individuals. It's important to discuss any changes or concerns with the treating psychiatrist. In the next section, we'll discuss potential side effects, drug interactions, and other important considerations when taking Lexapro. Potential Side Effects and Things to ConsiderStarting a new medication can be a source of concern for many people. Being aware of potential side effects and understanding how to manage them can help alleviate some of this anxiety. In this section, we'll explore the common side effects of Lexapro, address potential drug interactions, and discuss the importance of monitoring and communication during treatment. Side EffectsLet's begin with the side effects. While Lexapro is generally well-tolerated, it can cause some common side effects, including:
It's worth noting that these side effects are often mild and tend to decrease as the body adjusts to the medication. However, if side effects persist or become severe, it's important to consult with the prescribing psychiatrist, who may adjust the dosage or switch to a different medication. Drug InteractionsWhen it comes to drug interactions, Lexapro can interact with certain medications or substances, potentially leading to increased side effects or reduced effectiveness. Some notable interactions include:
It's essential to inform your psychiatrist about all medications, supplements, and substances being taken to minimize the risk of harmful interactions. Monitoring and CommunicationContinuous monitoring and communication are key while taking Lexapro. Patients should keep their psychiatrist informed about any changes in symptoms, side effects, or overall well-being. This information can help the psychiatrist adjust the treatment plan if necessary. Last but not least, it's important to be aware of potential withdrawal symptoms if Lexapro is discontinued. Stopping the medication abruptly can lead to symptoms such as dizziness, irritability, headaches, and nausea. To minimize these symptoms, the psychiatrist will typically recommend tapering off the medication gradually. In summary, being aware of Lexapro's potential side effects, drug interactions, and the importance of monitoring can help ensure a successful treatment experience. Open communication with the psychiatrist is crucial throughout the process. In the next and final section, we'll discuss alternative treatments for those who may be seeking other options to manage their depression or anxiety. Alternative or Supplemental TreatmentsWhile Lexapro can be an effective treatment for many individuals, it's important to remember that there are alternative or supplemental treatments available for managing depression and anxiety. In this section, we'll discuss therapy options, lifestyle changes, and other medications or supplements that can be considered as alternatives or complementary approaches to Lexapro. Therapy OptionsPsychotherapy can be an essential component of a comprehensive mental health treatment plan. Some evidence-based therapy options for depression and anxiety include:
Lifestyle ChangesLifestyle changes can also make a significant difference in managing symptoms of depression and anxiety. These changes may include:
Other Medications and SupplementsIn some cases, different types of medications or supplements may be more appropriate than Lexapro. These may include:
In conclusion, there are various alternative or supplemental treatments available for individuals seeking options beyond Lexapro. A combination of therapy, lifestyle changes, and potentially other medications or supplements can be tailored to an individual's specific needs. As always, it's important to consult with a psychiatrist to determine the most appropriate course of action. ConclusionIn conclusion, Lexapro is a widely prescribed and effective medication for treating depression and anxiety disorders. As an SSRI, it works by increasing serotonin levels in the brain, helping to improve mood and alleviate symptoms. However, it's important for patients and their families to be well-informed about potential side effects, drug interactions, and the timeline for the medication to take effect. Open communication with the treating psychiatrist is crucial throughout the entire treatment process, as each individual's response to Lexapro can vary. If Lexapro isn't the right fit, there are various alternative treatments available, including different types of therapy, lifestyle changes, and other medications or supplements. Ultimately, finding the most effective and well-tolerated treatment plan is a collaborative process between the patient and their mental health professional. By staying informed, maintaining open communication, and exploring different treatment options, individuals can take an active role in managing their mental health and working toward a brighter, healthier future.
Idaho's psychiatrist shortage is triggering a mental health crisis throughout the state, especially in rural areas where patients lack access to in-person psychiatric services. This blog post explores the factors driving the crisis and evaluates its damaging effects. We highlight the critical role of telemedicine in broadening access to high-quality specialist mental health care. Discover how you can navigate Idaho's psychiatrist shortage with telemedicine services such as those offered at Apraku Psychiatry.
Key Insights on Idaho's Psychiatrist Crisis
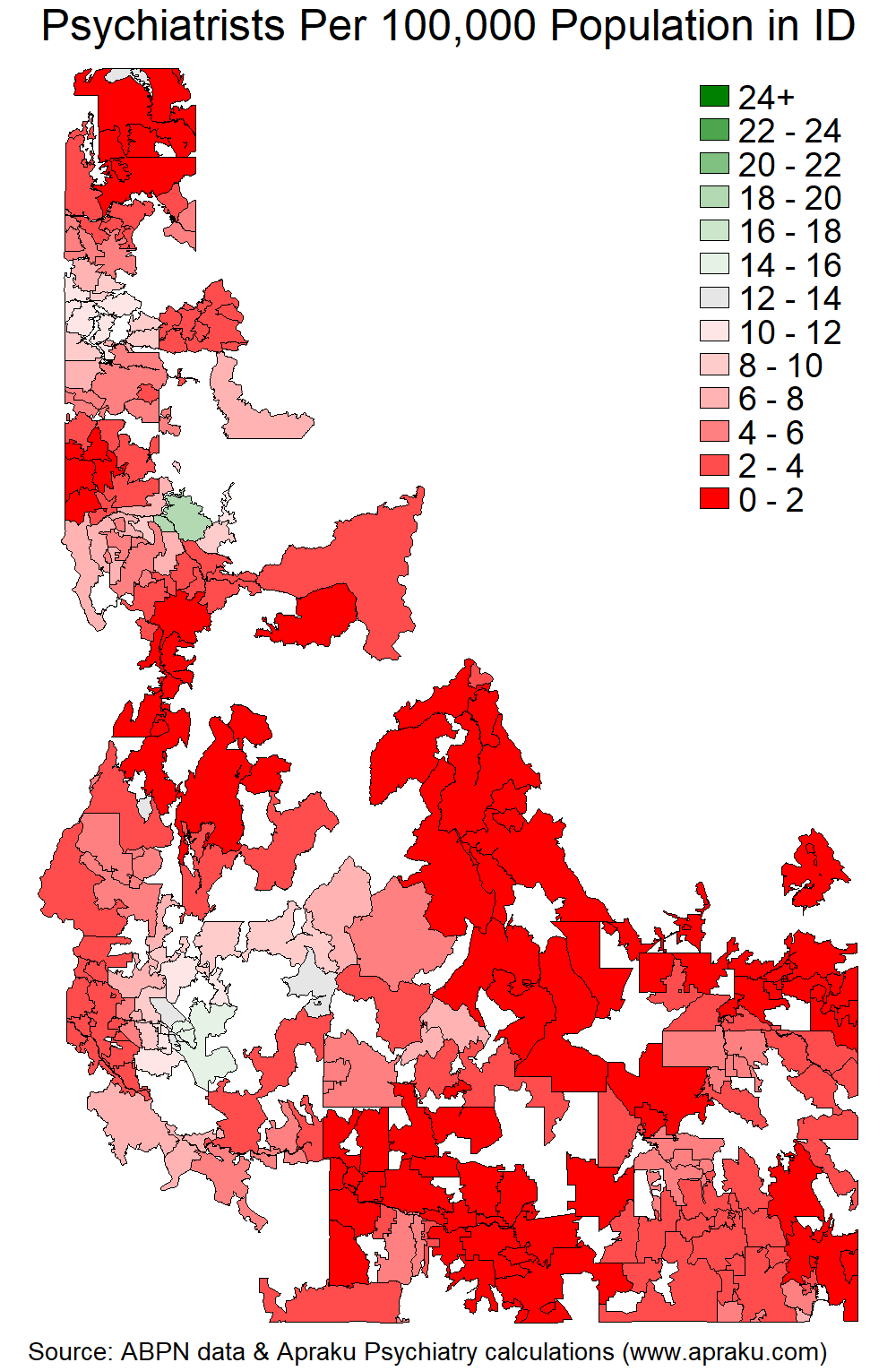
Overview of Idaho's Psychiatrist ShortageThe shortage of psychiatrists in Idaho is a critical issue that is affecting the mental health of the state's residents, especially in rural areas. The shortage has significant negative consequences for individuals, families, and communities, and addressing it is crucial for improving mental health outcomes in the state. Let’s start by taking a deeper dive into the numbers. With a population of nearly 2 million people, Idaho has fewer than 100 Board-certified psychiatrists, which translates to just 5 psychiatrists per 100,000 people. This is less than half the national average of 11 psychiatrists per 100,000 people and barely a third of what is considered adequate by the Department of Health and Human Services to meet the mental health needs of the population. The dearth of psychiatrists is especially acute in rural areas, where many residents are unable to access the mental health care they need. According to data from the American Board of Psychiatry & Neurology, most of Idaho's 44 counties have no psychiatrists at all. Unfortunately, the concentration of psychiatrists in Ada County, where more than half of Idaho's psychiatrists are located, only exacerbates the issue of limited access to mental health care for those outside the county. The Causes of Idaho's Psychiatrist ShortageThe shortage of psychiatrists in Idaho has been caused by three key factors, which have contributed to a lack of access to mental health care for residents in the state:
Effects of Idaho's Psychiatrist ShortageThe shortage of psychiatrists in Idaho has far-reaching consequences that affect individuals and communities. Patients seeking mental health care often face obstacles such as long wait times and limited transportation access, particularly in rural areas, which can lead to untreated mental health disorders. The situation is further complicated by Idaho's high suicide rate, one of the highest in the country. Without proper care, mental health disorders such as depression or bipolar disorder can worsen and lead to suicidal thoughts or attempts. Many individuals may not receive the necessary treatment or medication, leaving them vulnerable to further mental health decline. Additionally, some may resort to self-medication, resulting in substance abuse that only exacerbates mental health problems. In the absence of sufficient psychiatrists, many Idahoans turn to other providers, such as primary care physicians and nurse practitioners. While these providers play a vital role in the mental health care ecosystem, they lack the specialist training of psychiatrists. Primary care physicians may also have limited resources and support to treat complex mental health disorders, leading to delays in care and poor outcomes. The shortage of psychiatrists in Idaho has broader implications for communities, as untreated mental health disorders can lead to difficulties in daily activities such as employment, caring for loved ones, and basic self-care tasks. This can make it more challenging for individuals to access the resources necessary for recovery. The shortage of psychiatrists in Idaho therefore has significant negative consequences, highlighting the urgent need for solutions. Potential Solutions to Idaho's Psychiatrist ShortageTo effectively address the shortage of psychiatrists in Idaho, there are two main solutions.
Overall, both expanding the availability of psychiatric training programs and exploring telemedicine options can help to address the shortage of psychiatrists in Idaho. Telemedicine, in particular, offers an effective way to address access-to-care issues, especially in rural areas, and helps ensure that patients receive the mental health services they need, when they need them, regardless of their location in the state. ConclusionIdaho's psychiatrist shortage is a pressing issue that has far-reaching consequences for individuals, families, and communities. Expanding psychiatric training programs and leveraging telemedicine options are two vital solutions that can help alleviate this shortage. While both solutions have merit, telemedicine holds the most promise in the short term for addressing the shortage, as it can provide immediate access to psychiatric care for patients in Idaho, regardless of their location. Idahoans who experience difficulties accessing psychiatric care can consider making use of tele-psychiatry options, such as the Board-certified psychiatrists at Apraku Psychiatry. With appointments for new patients generally available within about a week, tele-psychiatry can be a game-changer for those in need of mental health care, bridging the gap caused by the shortage of psychiatrists in the state. This blog post is brought to you by Apraku Psychiatry. Apraku Psychiatry is a private practice offering video appointments with Board-certified psychiatrists licensed in multiple states. More blog articles can be found here. To schedule an appointment with one of our psychiatrists, patients can complete the online booking form.
Do you dread social situations? Is the idea of public speaking horrific, and does it feel like everyone is always watching and judging you? If so, you may be experiencing social anxiety.
When these symptoms are clinically significant, a psychiatrist may diagnose social anxiety disorder (SAD), which is a mental health condition that can leave people feeling isolated, lonely, and misunderstood. But the good news is that there are effective treatments available, and many people with SAD are able to manage their symptoms and lead fulfilling lives. In this blog post, we'll explore what SAD is, how to understand and process it, the different treatment options available, and ongoing management strategies. Whether you're struggling with SAD yourself or want to support a loved one, this post will provide valuable insights and practical tips. Understanding Social Anxiety DisorderDo you feel nervous meeting new people, giving presentations, or attending parties? If so, you're not alone. Many people experience some level of anxiety in social situations, but for some, social anxiety can be debilitating. In this section, we'll explore the difference between SAD and shyness, the challenges of underdiagnosis and undertreatment, and how to seek help for this treatable condition. The Difference Between SAD and ShynessSocial anxiety disorder (SAD) is often misunderstood and dismissed as just shyness or nervousness. However, while many people with SAD are shy or introverted, not all shy or introverted people have SAD. Shyness and introversion are common personality traits that don't necessarily interfere with daily life or cause significant distress. In contrast, SAD is a diagnosable condition that can significantly impair one's quality of life if left untreated. The Challenges of Underdiagnosis and UndertreatmentPeople with SAD experience extreme anxiety and self-consciousness in social situations, often fearing that they'll be judged or humiliated. Yet despite its prevalence and negative effects, SAD is often underdiagnosed and undertreated. Many people suffer in silence, feeling ashamed or embarrassed to seek help. However, getting help can make a significant difference in one's quality of life, and there's no shame in seeking it from a psychiatrist. In the next sections, we'll delve deeper into the symptoms and causes of SAD, as well as how to recognize them. Top Highlights
Causes of Social Anxiety DisorderNow we know what social anxiety disorder is, we might ask: what causes it? Like many mental health conditions, it's a combination of factors:
Recognizing Social Anxiety DisorderSAD is a complex condition that can manifest in a variety of ways, but there are some common symptoms to look out for. Here are some of the emotional, physical, and behavioral symptoms of SAD: Emotional Symptoms:
It's important to note that these symptoms can vary in severity and may not always be present. Some people with SAD may only experience symptoms in certain situations, while others may have a more generalized fear of all social situations. It's also important to differentiate SAD from other anxiety disorders, such as generalized anxiety disorder (GAD) or panic disorder. While these conditions share some similarities, they have different diagnostic criteria and treatment approaches. It's important to seek a professional diagnosis from a psychiatrist if you suspect you may have SAD or another anxiety disorder. If left untreated, SAD can have a significant impact on daily life. People with SAD may struggle to form meaningful relationships, perform well in school or work, or participate in activities they enjoy. They may also be at increased risk for other mental health conditions, such as depression or substance abuse. Evidence on the Prevalence of SAD
Treating Social Anxiety DisorderSocial anxiety disorder (SAD) can be a debilitating condition, but there are several effective treatments available, including medication, psychotherapy, and self-help strategies. While different treatments may work better for different people, medication can be an effective treatment option, particularly when used in combination with other treatments. In this section, we'll explore all the different types of interventions that can be used to treat SAD. MedicationMedication can be an effective treatment for social anxiety disorder. Different types of medications may be used to treat SAD, including:
PsychotherapyPsychotherapy can also be an effective treatment for social anxiety disorder. Different types of psychotherapy may be used to treat SAD, including:
Self-help strategiesIn addition to medication and psychotherapy, there are also a variety of self-help strategies that can be helpful for managing SAD. These strategies include:
Finding the right treatmentIt's important to note that treatment for SAD is not a one-size-fits-all approach. Different treatments may work better for different people, and it may take some trial and error to find the right combination of strategies. With the right treatment and support from a psychiatrist, many people with SAD are able to make significant improvements in their symptoms and quality of life. In the next section, we'll explore the prognosis and ongoing management of SAD, including relapse prevention and supporting loved ones. SSRIs as Effective Treatment for SAD
Prognosis and Management of Social Anxiety DisorderWhile social anxiety disorder (SAD) can be a chronic condition, many people are able to make significant improvements with proper psychiatric treatment and ongoing care in a supportive environment. Below are some strategies with proven effectiveness for ongoing management and relapse prevention. Ongoing ManagementManaging social anxiety disorder (SAD) over the long term can be challenging, but there are strategies that can be helpful for continuing treatment and reducing symptoms. Here are some key approaches:
Relapse PreventionWhile social anxiety disorder (SAD) symptoms may improve with treatment, they may still recur during times of stress or major life changes. Here are some strategies for preventing relapse:
Supporting Loved OnesFinally, if you have a loved one who is struggling with social anxiety disorder (SAD), there are several things you can do to offer support:
Empowering Interactions: Overcoming Social AnxietyThrough increased awareness, and by seeking professional help, individuals with social anxiety disorder can make significant strides towards a more fulfilling life. A tailored approach encompassing medication, psychotherapy, and self-help strategies has proven effective for many. In implementing these tips and insights, patients can effectively navigate their social interactions establish a robust support system. With commitment and persistence, those living with social anxiety disorder can overcome the challenges they face, ultimately enhancing their quality of life. Seeking help and working closely with a psychiatrist is an empowering step towards improved mental health and well-being. Embrace this journey with determination, and rediscover the joy of social connections. This blog post is brought to you by Apraku Psychiatry. Apraku Psychiatry is a private practice offering video appointments with Board-certified psychiatrists licensed in multiple states. More blog articles can be found here. To schedule an appointment with one of our psychiatrists, patients can complete the online booking form. |
Copyright © Apraku Psychiatry 2024